April 16, 2016-April 17, 2016
Presenter: Vivienne Rebel, MD, PhD
Associate Professor, Department of Cellular and Structural Biology, Health Science Center in San Antonio,
San Antonio, TX, United States of America
Abstract:
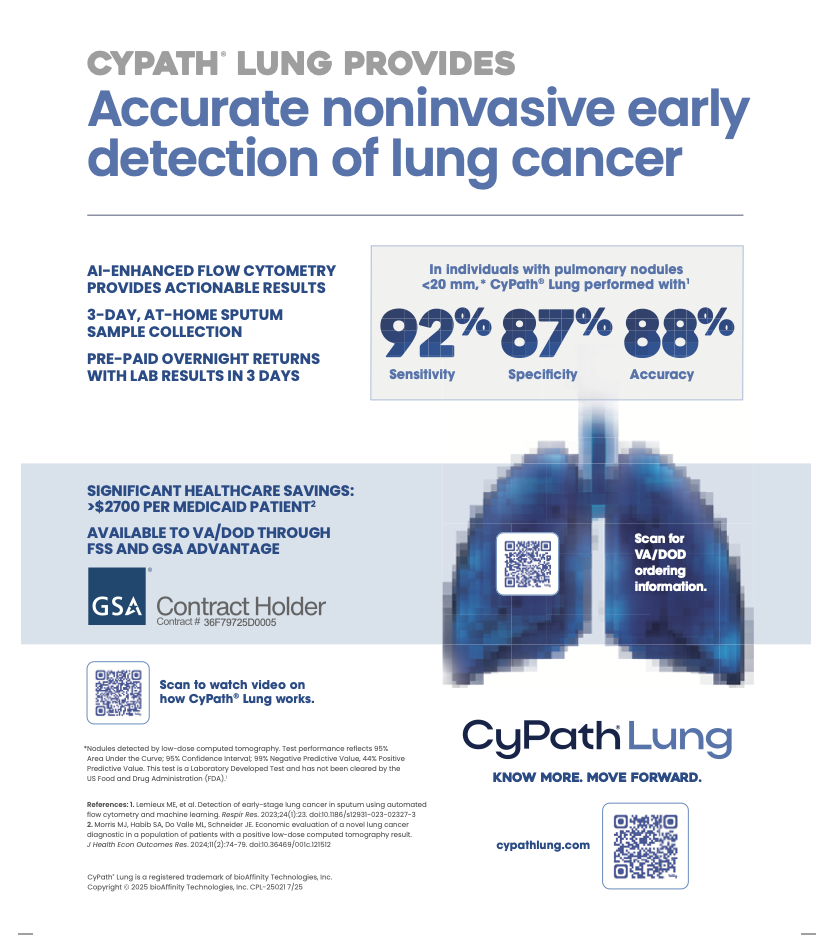
The overall 5-year survival rate of lung cancer in the United States is approximately 17%. This translates into more people dying in the U.S. from lung cancer alone than from prostate, breast or colon cancer combined. Lung cancer is the most common cancer worldwide. The high mortality rate of lung cancer is caused by the lack of early detection; indeed, studies have shown that if lung cancer is detected at Stage I, the 10-year survival rate is estimated to increase to 88% with treatment. Low-dose computed tomography (LDCT) is able to detect early-stage lung cancer with high sensitivity; however, the specificity of the procedure is low, resulting in a positive predictive value of less than 4%. Thus, for every 4 people correctly diagnosed with lung cancer, 96 will be incorrectly diagnosed and will be exposed to more LDCTs (radiation), biopsies and/or surgeries before they are correctly identified as lung cancer-free. The morbidity, mortality and enormous financial and emotional costs associated with the false-positive rate of LDCT have intensified the search for a new lung cancer detection assay that can be used as an adjunct to screening and significantly lower the false positive rate of LDCT alone. We recently developed a simple, non-invasive test to identify cancer cells in sputum of people with lung cancer. The test, based on a porphyrin-based labeling of deep-lung sputum, showed an overall accuracy of 81%, a false positive rate of 40% and a negative predictive value of 83% in a clinical trial that compared sputum collected from cancer patients (n=26) to that of high-risk (but no cancer) patients (n=102). None of the healthy volunteers, who were able to provide a deep-lung sputum sample (n=5) showed a positive test. Studies are currently underway to further improve clinical outcomes. It is well-established that porphyrins are taken up significantly more by cancer cells than by normal cells. However, the molecular mechanisms underlying this feature remain to be elucidated. We will discuss what is known in the literature about the cancer-specificity of porphyrins and what our own studies thus far have revealed.
is able to detect early-stage lung cancer with high sensitivity; however, the specificity of the procedure is low, resulting in a positive predictive value of less than 4%. Thus, for every 4 people correctly diagnosed with lung cancer, 96 will be incorrectly diagnosed and will be exposed to more LDCTs (radiation), biopsies and/or surgeries before they are correctly identified as lung cancer-free. The morbidity, mortality and enormous financial and emotional costs associated with the false-positive rate of LDCT have intensified the search for a new lung cancer detection assay that can be used as an adjunct to screening and significantly lower the false positive rate of LDCT alone. We recently developed a simple, non-invasive test to identify cancer cells in sputum of people with lung cancer. The test, based on a porphyrin-based labeling of deep-lung sputum, showed an overall accuracy of 81%, a false positive rate of 40% and a negative predictive value of 83% in a clinical trial that compared sputum collected from cancer patients (n=26) to that of high-risk (but no cancer) patients (n=102). None of the healthy volunteers, who were able to provide a deep-lung sputum sample (n=5) showed a positive test. Studies are currently underway to further improve clinical outcomes. It is well-established that porphyrins are taken up significantly more by cancer cells than by normal cells. However, the molecular mechanisms underlying this feature remain to be elucidated. We will discuss what is known in the literature about the cancer-specificity of porphyrins and what our own studies thus far have revealed.
PCS Global Cancer Conference – 2nd International Lung Cancer Symposium
Budapest, Hungary